Alzheimers/gut health link discovered
Lucy Kirk
25 July 2022, 8:55 PM
 A new discovery could be critical for preventing an avalanche of Alzheimer's disease.
A new discovery could be critical for preventing an avalanche of Alzheimer's disease.An exciting new discovery from Edith Cowan University (ECU) shows that getting your gut health right could play a big part in softening the projected $442 billion impact of Alzheimer’s disease on the Australian economy.
Alzheimer's Disease (AD) currently impacts an estimated 161,000 people in NSW alone, which Dementia Australia reports is a 'terrifying amount.' The disease, which currently has no known curative treatments, destroys memory and thinking ability and is the most prevalent form of dementia.
While dementia itself may not cause death, the result of progressive brain disorders is eventually fatal, and it's cost to the Australian economy is also debilitating.
Lead author of the report The Economic and Societal Cost of Alzheimer's Disease in Australia, 2021-2041, Emeritus Professor Laurie Brown from NATSEM, said the number of people aged 50 and over with diagnosed Alzheimer’s disease is expected to increase by 73% by 2041. This increase will lead to an annual cost of $26.6 billion.
“The modelling paints a significant challenge to government, health and aged care systems into the future,” said Professor Brown. “The numbers also provide insight into the ripple effect on families and the community as they struggle to care for people living with the disease.”
However, researchers from ECU say that the cost doesn't have to be so high. The team recently discovered that people with AD and gut disorders have genes in common - which is important for many reasons.
“The study provides a novel insight into the genetics behind the observed co-occurrence of AD and gut disorders,” research lead Dr Emmanual Adewuyi said.
“This improves our understanding of the causes of these conditions and identifies new targets to investigate to potentially detect the disease earlier and develop new treatments for both types of conditions.”
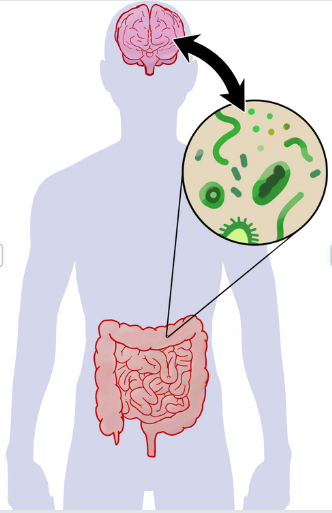
A confirmed genetic link between AD and multiple gut disorders "provides further evidence to support the concept of the ‘gut-brain’ axis, a two-way link between the brain’s cognitive and emotional centres, and the functioning of the intestines,” said Centre for Precision Health director and study supervisor Professor Simon Laws.
The discovery could lead to a new focus for dementia treatments.
Most interestingly, researchers found that abnormal levels of cholesterol were shown to be a risk for both AD and gut disorders.
“Looking at the genetic and biological characteristics common to AD and these gut disorders suggests a strong role for lipids metabolism, the immune system, and cholesterol-lowering medications,” said Dr Adewuyi.
“Whilst further study is needed into the shared mechanisms between the conditions, there is evidence high cholesterol can transfer into the central nervous system, resulting in abnormal cholesterol metabolism in the brain," he said.
Dementia Australia's Associate Professor and Honorary Medical Advisor, Michael Woodward, interpreted this research to suggest diet management as a key consideration for prevention.
"The best diet for preventing and slowing down the process of Alzheimer's disease is a Mediterranean diet – lots of vegetables and fruit, with very little oils and sweets and not too much red meat has proven to be the most effective for living longer," he said.
"There are numerous new approaches to understanding how AD occurs which is all very promising but we're not quite there yet. This means the best thing we can do to help ourselves is eat a proper diet and get plenty of exercise," said Dr Woodward.
Whilst further studies and analysis is needed, ECU have reported that the cholesterol link could be vital in treating AD in the future, potentially helping to suppress the economic and societal consequences that an increase in AD could cause, and giving hope to ageing Australians.




